How Lupus Can Affect the Feet

Lupus is an autoimmune disease that can affect the feet, often causing pain, swelling, and circulation problems. Inflammation from lupus may lead to joint damage, resulting in conditions such as Jaccoud’s arthropathy, where the toes become misaligned, making walking difficult. Polyarthritis can also develop, causing persistent stiffness and discomfort in the foot and ankle joints. Many people with lupus experience Raynaud’s phenomenon, which reduces blood flow to the toes, leading to cold, numb, or discolored feet. This condition can make standing or walking painful, especially in colder temperatures. Lupus may also cause sores or blisters on the feet to heal slowly, increasing the risk of infection. Nerve damage linked to lupus can result in tingling, burning sensations, or loss of feeling in the feet. A podiatrist can help manage these symptoms by evaluating your foot structure, addressing circulation concerns, and recommending treatments that improve mobility and reduce pain. In severe cases, surgery may be needed to correct deformities. If you have foot pain that may be related to lupus, it is suggested that you schedule an appointment with a podiatrist for an exam and appropriate treatment solutions.
When dealing with systemic disease of the feet, it is extremely important to check the affected areas routinely so that any additional problems are caught quickly. If you have any concerns about your feet and ankles contact our doctors from Foot & Ankle Center of Oklahoma. Our doctors will assist you with all of your podiatric needs.
Systemic Diseases of the Feet
Systemic diseases affect the whole body, and symptoms usually are displayed in the feet. This condition can make a patient’s ability to walk unbearable. Systemic diseases include gout, diabetes mellitus, neurological disorders, and arthritis.
Gout – is caused by an excess of uric acid in the body. Common symptoms include pain, inflammation, and redness at the metatarsal/phalangeal joint of the base big toe. Gout can be treated by NSAIDs to relieve pain and inflammation, and other drugs that lower the acid levels in the body.
Diabetes mellitus – is an increase in the level of blood sugar that the body cannot counteract with its own insulin. Failure to produce enough insulin is a factor in Diabetes.
Diabetes of the Feet
Diabetic Neuropathy – may lead to damaged nerves and affect the feet through numbness and loss of sensation.
Peripheral Vascular Disease – can restrict the blood flow to the feet, and often times lead to amputation of the feet.
If you have any questions please feel free to contact our offices located in Oklahoma City and Yukon, OK . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Systemic Diseases of the Foot
There are several systemic diseases, or diseases that affect the whole body, that either display symptoms in the feet or affect the health of the feet. Common systemic diseases that affect the overall health of the feet, and the patient’s ability to walk comfortably, include gout, diabetes mellitus, neurological disorders, and arthritis, among others.
In gout, which is caused by an excessive buildup of uric acid in the body, the most common symptoms of pain, inflammation, and redness occur at the metatarsal/phalangeal joint at the base of the big toe. Any excess levels of uric acid crystallize and are deposited in tendons, joints, and surrounding bone and muscle tissue. Gout is commonly treated with NSAIDs to relieve pain and inflammation and other drugs to lower uric acid levels in the body. Gout most commonly affects those who are overweight, have low protein diets and lead a more sedentary lifestyle.
Diabetes mellitus is an increase in the level of blood sugar in which the body cannot counteract with naturally occurring insulin in the body. The three types of diabetes, Type I, Type II and Gestational Diabetes, are all signs the body is either not producing enough insulin or is not efficiently using the insulin that is produced. Gestational diabetes only affects women who are pregnant and have never, prior to pregnancy, exhibited symptoms of the disease.
There are two main issues that affect the feet that are commonly caused by diabetes. They include diabetic neuropathy and peripheral vascular disease. Diabetic neuropathy can lead to damaged nerves and affect the feet through numbness and loss of sensation. Peripheral vascular disease restricts the flow of blood to the foot and can, in extreme cases, lead to the necessity of amputating the foot. Peripheral issues that are caused by diabetes and can affect the foot include athlete’s foot, nail infections, corns, blisters, bunions, severe dry skin, plantar warts and ingrown toenails. These can all be attributed to the decrease of blood flow to the foot.
Neurological disorders and rheumatoid arthritis can also have severe impact on the health of the feet. Neurological disorders can affect the nerves in the main structure of the foot and cause loss of sensation and possible decreased muscle response. Rheumatoid arthritis can affect the bones and joint structures of the foot, making it impossible to walk normally without serious pain.
All systemic diseases that affect the foot can effectively be treated to minimize joint and muscle damage if they are diagnosed early and treated with medication and lifestyle therapy. Diabetes patients must monitor their blood sugar levels and work with their physician to keep their levels as close to normal as possible. Rheumatoid arthritis patients should work with their physician to ensure the proper medications are being taken to reduce the amount of damage to the joints of the body.
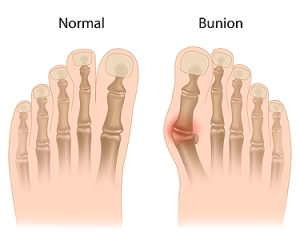
Managing Bunions
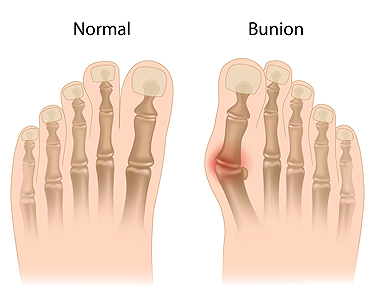
A bunion is a bony bump that forms at the base of the big toe, as the top of the toe angles toward the inner toes. This misalignment can lead to pain, swelling, and redness surroundig the joint. Over time, bunions may become more noticeable, with the bump growing larger and causing the skin to thicken or develop corns. Bunions are often caused by genetics, but factors like wearing tight shoes, high heels, or arthritis can also contribute. Symptoms include pain when walking, tenderness, and difficulty in finding comfortable shoes. Treatment options range from non-surgical to surgical solutions. A podiatrist can recommend changes to footwear, custom orthotics, and targeted exercises to ease pain and improve foot alignment. In more severe cases, surgery may be necessary to realign the toe and remove the bony bump. If you have a bunion causing discomfort or affecting your mobility, a podiatrist can provide personalized care. It is suggested that you schedule an appointment to explore your best treatment options.
If you are suffering from bunion pain, contact our doctors of Foot & Ankle Center of Oklahoma. Our doctors can provide the care you need to keep you pain-free and on your feet.
What Is a Bunion?
Bunions are painful bony bumps that usually develop on the inside of the foot at the joint of the big toe. As the deformity increases over time, it may become painful to walk and wear shoes. Women are more likely to exacerbate existing bunions since they often wear tight, narrow shoes that shift their toes together. Bunion pain can be relieved by wearing wider shoes with enough room for the toes.
Causes
- Genetics – some people inherit feet that are more prone to bunion development
- Inflammatory Conditions - rheumatoid arthritis and polio may cause bunion development
Symptoms
- Redness and inflammation
- Pain and tenderness
- Callus or corns on the bump
- Restricted motion in the big toe
In order to diagnose your bunion, your podiatrist may ask about your medical history, symptoms, and general health. Your doctor might also order an x-ray to take a closer look at your feet. Nonsurgical treatment options include orthotics, padding, icing, changes in footwear, and medication. If nonsurgical treatments don’t alleviate your bunion pain, surgery may be necessary.
If you have any questions, please feel free to contact our offices located in Oklahoma City and Yukon, OK . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Bunions
A bunion is a bump that forms at the base of the big toe. Bunions form when the big toe pushes against the next toe, which forces the big toe joint to get bigger and stick out. As a result, the skin over the bunion may start to appear red and it may feel sore.
There are risk factors that can increase your chances of developing bunions. People who wear high heels or ill-fitting shoes are more likely to develop them, in addition to those who have a genetic history of bunions or have rheumatoid arthritis.
The most obvious way to tell if you have a bunion is to look for the big toe pushing up against the toe next to it. Bunions produce a large protrusion at the base of the big toe and may or may not cause pain. Other symptoms are redness, swelling, and restricted movement of the big toe if you have arthritis.
Nonsurgical methods are frequently used to treat bunions that aren’t severe. Some methods of nonsurgical treatment are orthotics, icing and resting the foot, taping the foot, and pain medication. Surgery is usually only required in extreme cases. However, if surgery is needed, some procedures may involve removing the swollen tissue from around the big toe joint, straightening the big toe by removing part of the bone, or joining the bones of your affected joint permanently.
Your podiatrist will diagnose your bunion by doing a thorough examination of your foot. He or she may also conduct an x-ray to determine the cause of the bunion and its severity.
How Seed Corns Develop

Seed corns, also known as a seed corn wart, is a type of corn that forms on the bottom of the foot, often near the toes or on the ball of the foot. It is a thickened area of skin caused by repeated pressure or friction, leading to the accumulation of dead skin cells. The term seed corn refers to the small, hard center of the corn that can resemble a seed. These growths develop when the skin tries to protect itself from constant irritation, such as from wearing tight shoes, abnormal foot mechanics, or walking habits that place excessive pressure on certain areas of the foot. Over time, the body builds up extra skin in response, forming a hard, raised bump. While seed corns are not usually painful, they can cause discomfort when pressure is applied. Corns can be a bothersome foot condition. If you have developed any type of corn on your foot, it is suggested that you consult a podiatrist who can offer you effective relief and prevention tips.
Corns can make walking very painful and should be treated immediately. If you have questions regarding your feet and ankles, contact our doctors of Foot & Ankle Center of Oklahoma. Our doctors will treat your foot and ankle needs.
Corns: What Are They? And How Do You Get Rid of Them?
Corns are thickened areas on the skin that can become painful. They are caused by excessive pressure and friction on the skin. Corns press into the deeper layers of the skin and are usually round in shape.
Ways to Prevent Corns
There are many ways to get rid of painful corns such as:
- Wearing properly fitting shoes that have been measured by a professional
- Wearing shoes that are not sharply pointed or have high heels
- Wearing only shoes that offer support
Treating Corns
Although most corns slowly disappear when the friction or pressure stops, this isn’t always the case. Consult with your podiatrist to determine the best treatment option for your case of corns.
If you have any questions please feel free to contact our offices located in Oklahoma City and Yukon, OK . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Understanding Corns and Calluses
Corns and Calluses are both hardened layers of thickened skin that develop because of friction. Both ailments are typically found on the feet and may be unsightly. Although they have similarities, corns and calluses are different from each other.
Some causes of corns and calluses may be wearing ill-fitting shoes and not wearing socks. If you wear tight shoes, your feet will constantly be forced to rub against the shoes, causing friction. If you fail to wear socks, you are also causing your feet to endure excess friction.
There are some signs that may help you determine whether you have one of these two conditions. The first symptom is a thick, rough area of skin. Another common symptom is a hardened, raised bump on the foot. You may also experience tenderness or pain under the skin in addition to flaky, dry, or waxy skin.
There are also risk factors that may make someone more prone to developing corns and calluses. If you are already dealing with bunions or hammertoe, you may be more vulnerable to having corns and calluses as well. Other risk factors are foot deformities such as bone spurs, which can cause constant rubbing inside the shoe.
Corns tend to be smaller than calluses and they usually have a hard center surrounded by inflamed skin. They also tend to develop on the parts of the body that don’t bear as much weight such as the tops and sides of toes. Corns may also be painful for those who have them. On the other hand, calluses are rarely painful. These tend to develop on the bottom of the feet and may vary in size and shape.
Fortunately, most people only need treatment for corns and calluses if they are experiencing discomfort. At home treatments for corns and calluses should be avoided, because they will likely lead to infection. If you have either of these ailments it is advised that you consult with your podiatrist to determine the best treatment option for you.
Ankle-Foot Orthoses for Stroke Patients

Ankle-foot orthoses, or AFOs, can help stroke survivors improve their walking ability. They are devices worn on the lower leg and foot to support movement. Passive AFOs provide stability and hold the foot in a fixed position to prevent dragging and tripping. Dynamic AFOs, on the other hand, offer more flexibility, allowing smoother motion during walking. These devices are especially helpful for individuals with plantar flexor, or lower leg muscle weakness, which are involved in the push-off phase of walking. By improving alignment and control, AFOs make walking easier and safer, reducing the risk of falls. Each type of AFO is designed to address different needs, so the right choice depends on the individual. If you have had a stroke and want to improve your walking ability, it is suggested that you schedule an appointment with a podiatrist who can assess your condition, recommend the most suitable orthotic, and ensure it fits comfortably for the best results.
If you are having discomfort in your feet and would like to try orthotics, contact our doctors from Foot & Ankle Center of Oklahoma. Our doctors can provide the care you need to keep you pain-free and on your feet.
What Are Orthotics?
Orthotics are inserts you can place into your shoes to help with a variety of foot problems such as flat feet or foot pain. Orthotics provide relief and comfort for minor foot and heel pain but can’t correct serious biomechanical problems in your feet.
Over-the-Counter Inserts
Orthotics come in a wide variety of over-the-counter inserts that are used to treat foot pain, heel pain, and minor problems. For example, arch supports can be inserted into your shoes to help correct overarched or flat feet, while gel insoles are often used because they provide comfort and relief from foot and heel pain by alleviating pressure.
Prescription Orthotics
If over-the-counter inserts don’t work for you or if you have a more severe foot concern, it is possible to have your podiatrist prescribe custom orthotics. These high-quality inserts are designed to treat problems such as abnormal motion, plantar fasciitis, and severe forms of heel pain. They can even be used to help patients suffering from diabetes by treating foot ulcers and painful calluses and are usually molded to your feet individually, which allows them to provide full support and comfort.
If you are experiencing minor to severe foot or heel pain, it’s recommended to speak with your podiatrist about the possibilities of using orthotics. A podiatrist can determine which type of orthotic is right for you and allow you to take the first steps towards being pain-free.
If you have any questions please contact our offices located in Oklahoma City and Yukon, OK . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Foot Orthotics
Orthotics are shoe inserts that are meant to correct an irregular walking gait or provide cushioning to the feet. Orthotics come in a variety of different models and sizes, including over-the-counter and customizable variants. Customizable orthotics can be shaped and contoured to fit inside a specific shoe and are typically prescribed through a podiatrist who specializes in customized footwear and orthotics design and management.
Orthotics are beneficial because they can help prevent injuries from occurring and provide cushioning to keep pain levels down to a minimum. They also allow for the correct positioning of the feet. Orthotics can act as shock absorbers to help remove pressure from the foot and ankle. Therefore, orthotics can make bodily movements, such as walking and running, become more comfortable as well as help prevent the development of certain foot conditions.
Orthotics alleviate pain and make the foot more comfortable by slightly altering the angle at which the foot strikes the ground surface, therefore controlling the movement of the foot and ankle. Orthotics come in different variants and can be made of various materials. To determine what type of orthotic is most suited to your feet and your needs, it is best to consult your podiatrist. He or she will be able to recommend a type of orthotic that can help improve your foot function or prescribe a custom orthotic to best fit your feet.
Get Professional Care for a Broken Foot or Ankle
Diabetic Wound Care

Diabetic wounds, particularly on the feet, are a serious concern for people with diabetes due to reduced blood flow and nerve damage. These wounds can develop from minor cuts, blisters, or pressure sores and may not heal properly due to poor circulation and neuropathy. Additionally, sometimes diabetic wounds do not engage the immune cells necessary for normal wound healing. Symptoms include redness, swelling, pain, or the presence of an open sore that does not heal over time. In some cases, the wound may become infected, causing increased pain, warmth, or drainage. The main causes of diabetic wounds include high blood sugar, which affects circulation and immune response, as well as nerve damage that reduces sensitivity to pain. Treatment typically involves thorough cleaning, wound dressings, and possibly antibiotics for infection. A podiatrist can provide specialized care, including debridement, tips on custom footwear, and guidance on managing blood sugar to prevent further complications. If you have diabetes and have developed a foot wound, it is suggested that you schedule an appointment with a podiatrist.
Wound care is an important part in dealing with diabetes. If you have diabetes and a foot wound or would like more information about wound care for diabetics, consult with our doctors from Foot & Ankle Center of Oklahoma. Our doctors will assess your condition and provide you with quality foot and ankle treatment.
What Is Wound Care?
Wound care is the practice of taking proper care of a wound. This can range from the smallest to the largest of wounds. While everyone can benefit from proper wound care, it is much more important for diabetics. Diabetics often suffer from poor blood circulation which causes wounds to heal much slower than they would in a non-diabetic.
What Is the Importance of Wound Care?
While it may not seem apparent with small ulcers on the foot, for diabetics, any size ulcer can become infected. Diabetics often also suffer from neuropathy, or nerve loss. This means they might not even feel when they have an ulcer on their foot. If the wound becomes severely infected, amputation may be necessary. Therefore, it is of the upmost importance to properly care for any and all foot wounds.
How to Care for Wounds
The best way to care for foot wounds is to prevent them. For diabetics, this means daily inspections of the feet for any signs of abnormalities or ulcers. It is also recommended to see a podiatrist several times a year for a foot inspection. If you do have an ulcer, run the wound under water to clear dirt from the wound; then apply antibiotic ointment to the wound and cover with a bandage. Bandages should be changed daily and keeping pressure off the wound is smart. It is advised to see a podiatrist, who can keep an eye on it.
If you have any questions, please feel free to contact our offices located in Oklahoma City and Yukon, OK . We offer the newest diagnostic and treatment technologies for all your foot care needs.